Intensive Care
Supporting Critical Care for Adult and Paediatric ICU Patients
Home / ICU and PICU
ICU and PICU
Effectively monitoring intensive care patients can be challenging. Adding to the challenge, it can be difficult for clinicians to quickly assess a deteriorating patient as ICU rooms are often cluttered with multiple disparate monitors. Masimo’s advanced intensive care monitoring solutions equip clinicians with an integrated, centralised display of multiple noninvasive measurements and EMR integration to automate transcription of medical events – which may facilitate quicker awareness of changing patient conditions.
Real-time Measurements
Real-time Measurements
While invasive blood draws are routinely conducted in the ICU, there is a lack of visibility to a patient’s haemoglobin status between intermittent laboratory results. Noninvasive and continuous SpHb® can provide real-time visibility to changes, or lack of changes, in haemoglobin between invasive blood samples. For example, SpHb monitoring may provide insight when the haemoglobin trend is dropping and the clinician may otherwise think haemoglobin is stable.
Improper titration of fluid can lead to hypovolemia or hypervolemia that may be associated with negative outcomes.1 Pleth Variability Index (PVi®), a noninvasive dynamic parameter that helps clinicians monitor fluid responsiveness in mechanically-ventilated patients, measures the dynamic changes in Perfusion Index (Pi) that occur during the respiratory cycle. When monitored together, SpHb and PVi may provide clinicians with additional insight into a patient's status.
The rainbow SET platform, including SpHb and PVi, can be integrated into existing ICU multi-parameter monitors, such as the Philips IntelliVue MX800, to help simplify clinician workflows.

A More Complete Picture of the Brain
A More Complete Picture of the Brain

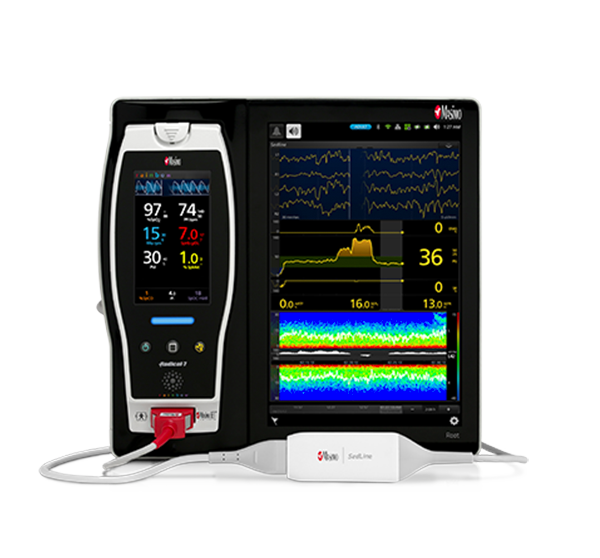
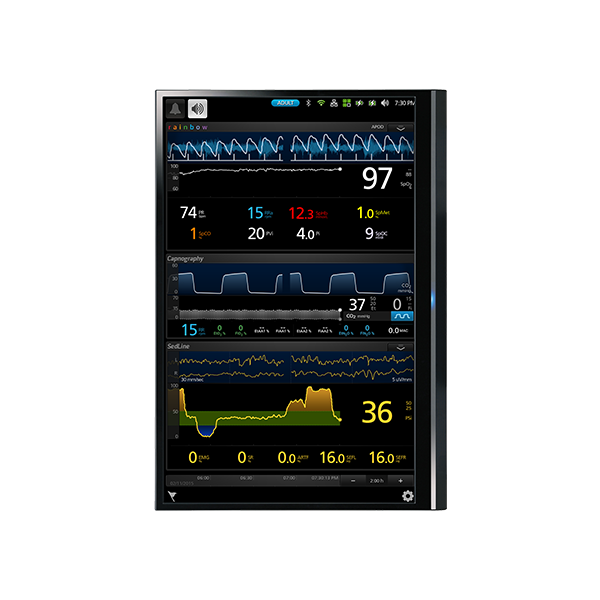
Anaesthesia and sedation are utilised in many surgical and intensive care scenarios, but the over- and under-administration of agents is common.2,3,4 Next Generation SedLine® brain function monitoring helps clinicians monitor the state of the brain under anaesthesia with bilateral acquisition and processing of four leads of electroencephalogram (EEG) signals. Next Generation SedLine features an enhanced signal processed EEG index (PSi) with less susceptibility to EMG interference and improved performance in low power EEG cases, as well as an enhanced Multitaper Density Spectral Array (DSA).
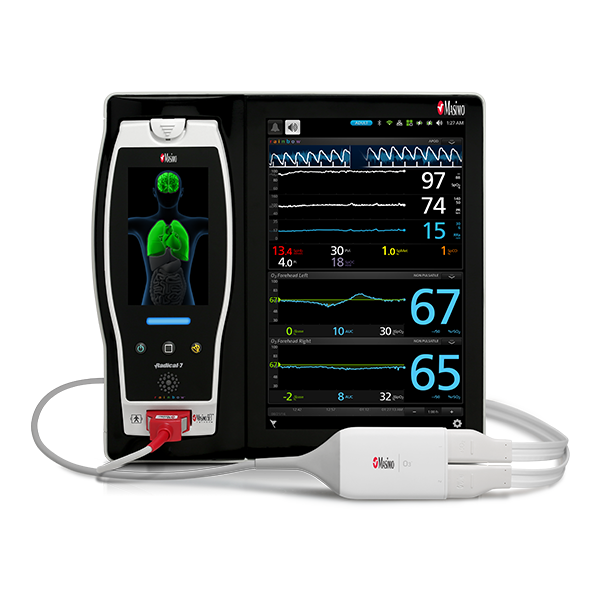
Next Generation SedLine can be used simultaneously with O3® regional oximetry on the Root® platform for a more complete picture of the brain. O3 may help clinicians monitor cerebral oxygenation in situations in which pulse oximetry alone may not be fully indicative of the oxygen in the brain.
Integrated Respiratory Monitoring
Integrated Respiratory Monitoring
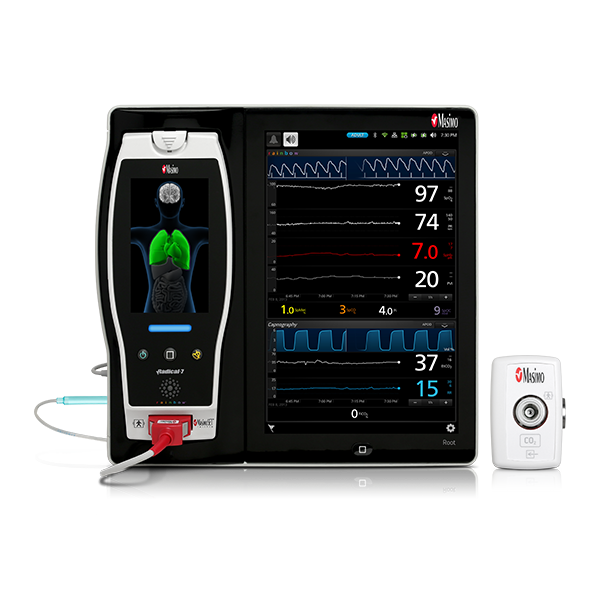
The Anaesthesia Patient Safety Foundation (APSF) states that continuous electronic monitoring of oxygenation and ventilation should be available and considered for all patients during the post-operative period to reduce the likelihood of unrecognised clinically significant opioid-induced depression of ventilation.5 Hypoventilation, hyperventilation, airway obstruction, and other potentially life-threatening conditions can be rapidly detected with capnography – providing clinicians with valuable data that may allow them to intervene earlier.6
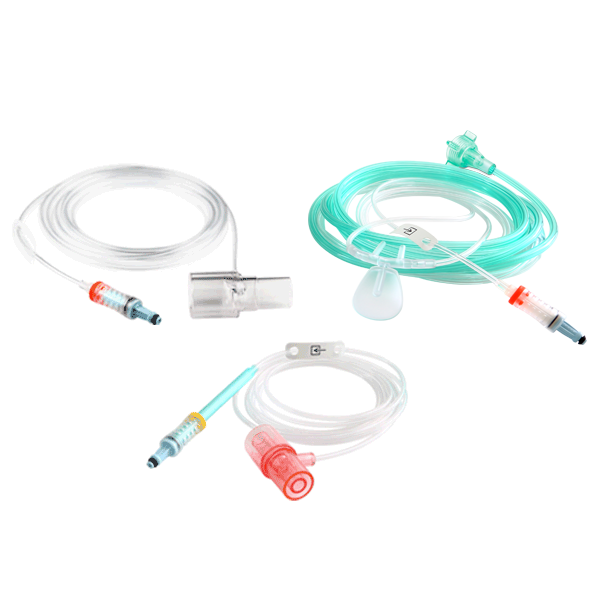
Masimo NomoLine™ capnography provides sidestream CO2 and gas monitoring with a wide variety of sampling lines for intubated and non-intubated adult, paediatric, and neonatal patients. NomoLine capnography seamlessly integrates into Root with Masimo SET® pulse oximetry and other key physiologic parameters, providing clinicians with greater visibility to a patient’s oxygenation, ventilation, and respiratory status.
Masimo also offers rainbow Acoustic Monitoring® (RAM®), a noninvasive and continuous method of monitoring respiratory rate in post-operative patients that has the benefit of higher patient compliance.7,8 For patients who don’t require CO2 monitoring, RAM offers clinicians the flexibility of choosing the most applicable respiration monitoring method for each patient.

Advanced Patient Monitoring and Connectivity Platforms
Advanced Patient Monitoring and Connectivity Platforms
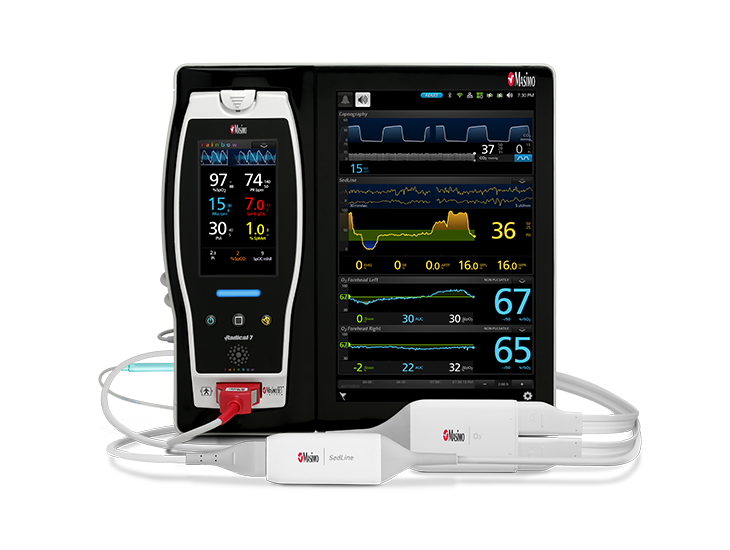
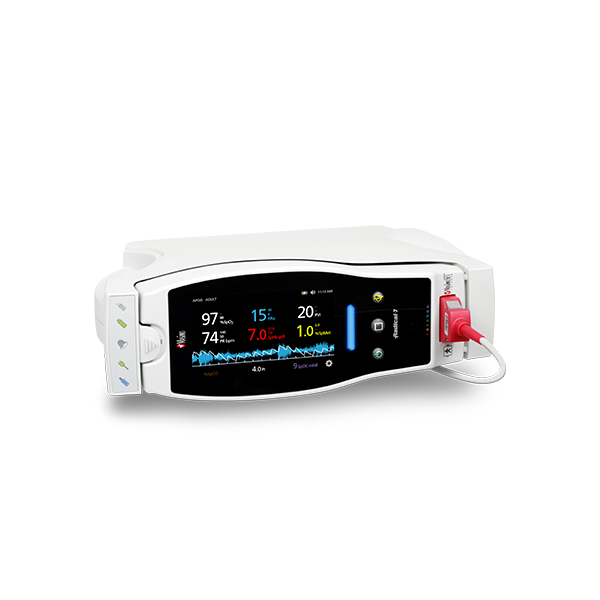
Masimo’s critical care monitoring solutions are available together on Root, a highly customisable, expandable patient monitoring and connectivity platform that occupies a minimal footprint in the ICU. Compact yet powerful, Root provides multiple high-impact, innovative measurements on a single platform, replacing many larger monitors in a cluttered environment and providing clinicians with more information in one place.
Iris Gateway™ and Iris® ports on Root facilitate automated data transfer from Root and multiple third-party standalone monitors — such as IV pumps, ventilators, and anaesthesia machines – to hospital EMRs, in addition to other databases or third party displays, which may reduce the likelihood of transcription errors9 or incomplete case records.
Measurements
Measurements
Intensive Care Solutions
References:
- 1.
Bellamy et al. Br J Anaesth. 2006.
- 2.
Hughes, C. G. et al. Clinical Pharmacology: Advances and Applications. 2012;4:53-63.
- 3.
Jackson DL et al. Crit Care. 2009;13(6):R204.
- 4.
Simpson, Jeffrey R. et al. The American Surgeon. 79, no. 10 (2013): 1106-1110.
- 5.
Matthew B. Weinger and Lorri A. Lee for the Anesthesia Patient Safety Foundation. “No Patient Shall Be Harmed By Opioid-Induced Respiratory Depression.” Volume 26, No. 2, 21-40. Retrieved from https://www.apsf.org/newsletters/pdf/fall_2011.pdf.
- 6.
Nagler J et al. Emerg Med Clin North Am. 2008 Nov;26(4):881-97.
- 7.
Macknet MR et al. Anesthesiology. 2007;107:A84. (abstract).
- 8.
Goudra BG et al. Open J Anesthesiol. 2013; 3:74-79.
- 9.
The Value of Medical Device Interoperability. West Health Institute. 2013.
RESOURCES
SpHb monitoring is not intended to replace laboratory blood testing. Blood samples should be analysed by laboratory instruments prior to clinical decision making.
For professional use. See instructions for use for full prescribing information, including indications, contraindications, warnings, and precautions.
PLCO-002024/PLM-11355A-0718